
P: (08)9965 0697 F: (08)9964 7528
News
Heart Week 2014 Sunday 4 May - Saturday 10 May 2014 May 5th, 2014
8 Ways to Prevent Sprains & Strains in the Workplace May 4th, 2014
50% of worksite injuries are sprains and strains are the greatest cause of workplace injury.
In the workplace most of these types of injuries are caused by manual tasks such as lifting or carrying loads, working in fixed positions, repetitive tasks or using heavily vibrating toolsThe second greatest cause of sprains and strains is slips, trips and falls at ground level and from heights such as jumping from vehicles, which can cause lower limb and back strains.
While some workplace hazards are easy to spot like a missing guard on a saw or a bucket in the middle of a busy shop floor sprains and strains are not always that obvious. This is because they can be caused by the way work is designed and carried out like awkward body posture, high body force and high task repetition that is more insidious.
1. Recognise the Signs – Aches, Become Pains, Become Injuries
Often musculoskeletal injury comes with warning signs and symptoms before an injury occurs, and long before any work is missed. Review the incident reports, listen to your workforce and keep an eye out for things like:
- Comments about discomfort or pain
- Stretching or rubbing muscles while working
- Repetitive similar injuries with specific tasks
- High turnover or absenteeism in a particular section
2. Consult about Musculoskeletal Hazards
Talk to workers about the most difficult parts of the job like holding awkward body postures and doing highly repetitive work for extended periods and find a better way together. Workers who are doing the job are generally best placed to find solutions.
3. Fix the Hazards
Consider what improvements could be made to the way work is done to improve working posture such as the position of the work or change the workstation layout to eliminate excessive reaching or leaning forward. Next time you go through a checkout look at the workstation layout and I am sure you will see the risks.
Position frequently used tools and equipment within easy reach and consider adjustable tables to accommodate everyone. Likewise reduce manual handling by using mechanical lifts to support and to move heavy loads and try to eliminate the lift by changing how objects are stored. Reducing the physical force and task repetition needed to do the job should be another focus.
Poor health contributes to the risk of strains and sprains. Workplace health promotion has a role in improving emplyee resilience
4. Consider Individual Factors.
It’s important to take care of the entire body with exercise, proper posture, a sensible diet and adequate rest. Injury is less likely in a worker who is physically fit than someone whose muscles or ligaments have weakened over time from lack of exercise or age. Smoking and fatigue are also issues that impact the wear and tear on a body.
Promote individual physical fitness and healthy living through a company wellness program. Think about introducing stretching before and during work to warm-up muscles and help relieve strain. Provide training and coach workers frequently on how to move material safety using lifting equipment and safe postures.
5. Focus on Ergonomic Design
Ergonomics is the match between design, the environment and the individual. It is not a one size fits all. It allows quality work to be completed safely and easily by fitting the job to the worker and providing appropriate equipment. For example someone who is taller needs a different chair to someone below average height.
6. Look at Organisational Hazards
If there is poor communication and organizational cooperation and limited worker involvement in decisions that affect working tasks then this will be reflected in a poor corporate culture, low worker morale and higher time lost and costs associated with sprains and strains such as workers’ compensation premium.
7. Find Workplace Champions
Active OHS can help you address the risks in your workplace. It’s hard to effect change on your own. It’s a Pantene thing it won’t happen overnight but it will happen if you have the right tools and support. Having workplace wellness champions can assist with raising overall awareness of the health, safety and welfare of the workforce by providing general information to colleagues as well as providing specific details on workplace risks and the support and assistance that is available to effect change.
8. Are you winning?
Set some Benchmarks. How does your workers’ compensation premium compare to other businesses in your industry? Where do you sit when it comes to sprains and strains?
If you aren't winning our IMS Assessment is inexpensive and can help highlight areas of need. Contact us for more
Reducing just six risk factors could prevent 37 million deaths from chronic diseases over 15 years May 3rd, 2014
Reducing or curbing just six modifiable risk factors -- tobacco use, harmful alcohol use, salt intake, high blood pressure and blood sugar, and obesity -- to globally-agreed target levels could prevent more than 37 million premature deaths over 15 years, from the four main non-communicable diseases (NCDs; cardiovascular diseases, chronic respiratory disease, cancers, and diabetes) according to new research published in The Lancet.
Worryingly, the findings indicate that not reaching these targets would result in 38.8 million deaths in 2025 from the four main NCDs, 10.5 million deaths more than the 28.3 million who died in 2010. This is the first study to analyse the impact that reducing globally targeted risk factors will have on the UN's 25x25 target to reduce premature deaths from NCDs by 25% relative to 2010 levels by 2025.
Using country-level data on deaths and risk factors and epidemiological models, Professor Majid Ezzati from Imperial College London, UK, and colleagues estimate the number of deaths that could be prevented between 2010 and 2025 by reducing the burden of each of the six risk factors to globally-agreed target levels -- tobacco use (30% reduction and a more ambitious 50% reduction), alcohol use (10% reduction), salt intake (30% reduction), high blood pressure (25% reduction), and halting the rise in the prevalence of obesity and diabetes.
Overall, the findings suggest that meeting the targets for all six risk factors would reduce the risk of dying prematurely from the four main NCDs by 22% in men and 19% for women in 2025 compared to what they were in 2010. Worldwide, this improvement is equivalent to delaying or preventing at least 16 million deaths in people aged 30-70 years and 21 million in those aged 70 years or older over 15 years.
Writing in a linked Comment, Professor Rifat Atun from Harvard School of Public Health, Harvard University, Boston, MA, USA says, "With political will and leadership, the 25×25 targets are well within reach. But despite robust evidence, well-proven cost-effective interventions, and a compelling case for action made by [this study] to address risk factors for NCDs to save millions of lives, political apathy prevails. Even with much discourse, meaningful and durable action against NCDs is scarce, with little accountability to achieve the promises made and the targets set at the General Assembly in 2011.
Complete our Free LifeRISK score to find out how many risk factors you have.
Obesity Surgery - Pre-Surgical Nutrition May 2nd, 2014
Many people waiting obesity surgery do not realise that the aim of the band is to sharply reduce food consumption. Preoperative education should include eating, psychological implications and risks and disadvantages of obesity surgery. Our registered dietitian can help patients make informed decisions.
People considering bariatric surgery must begin with preoperative weight loss using very low calorie diet (VLCD) meal replacements and low energy foods for 2—6 weeks. Some weight loss before the surgery reduces liver size and visceral and subcutaneous adiposity, making stomach access during surgery that much easier, minimising operative risks and length of surgery.
Our dietitian encourages the Optifast approach as the most evidence based VLCD.
Click for Handout
Introducing restrictive eating practices early also means patients understand what is required post-surgery. The length of this preoperative diet may depend on the patient’s initial weight and the maximum weight hospital and surgery beds can safely manage.
A preoperative assessment of nutrient markers is recommended with sufficient time to correct nutritional deficiencies. Despite their well-nourished appearance, these patients are often found to be deficient in nutrients such as folate, iron, selenium vitamin B12 and vitamin D. Vitamin D may be low due to reduced sunlight cutaneous synthesis and modest dress.
Preoperative nutrient defeciencies can be caused by poor diet choices, chronic dieting and medication side-effects. This pre-screening is also useful to distinguish post-surgery complications and biochemical changes.
Reference:
http://www.medicalobserver.com.au/news/banding-to-help-the-obese
Obesity Surgery - Post-Surgical Nutrition May 2nd, 2014
For the first two months the goals of postoperative nutrition care are to maintain adequate hydration; to correct and maintain nutrient status, including vitamins, minerals and protein, which are needed for healing; and to return gradually to normal food consistency.
Consistency begins with a liquid diet for the first 1—2 weeks, followed by puréed and soft foods for 2—4 weeks, and then smaller serves of normal foods. Progression through each texture will depend on the patient’s tolerance, and formulated products may be required. Nutritional deficiencies can still occur though from poorly tolerated foods and food consistencies, and unusual diets.
It is important for you to be psychological ready for this change in diet habits, as some patients continue dysfunctional eating of energy-dense, nutrient-poor foods — just in smaller portions.
Lifelong changes in eating behaviour are required, depending on the procedure, such as eating regular, but much smaller meals, eating more slowly, cutting food into small pieces and chewing well, and avoiding filling up on liquids. Frequent testing of nutrient markers is required every six months in the first 1—2 years.
An exercise program is also a necessary part of the postoperative routine. Along with diet compliance, exercise helps prevent weight regain and maintain weight loss.
Reference:
Safety First - Reduce UV Apr 30th, 2014
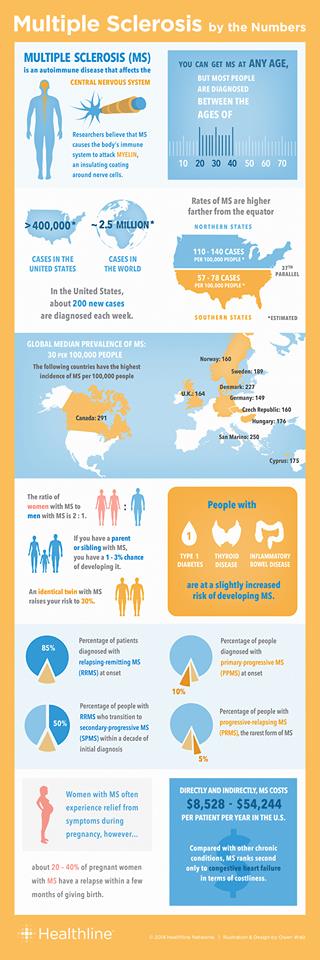
Infographic - Multiple Sclerosis Apr 30th, 2014
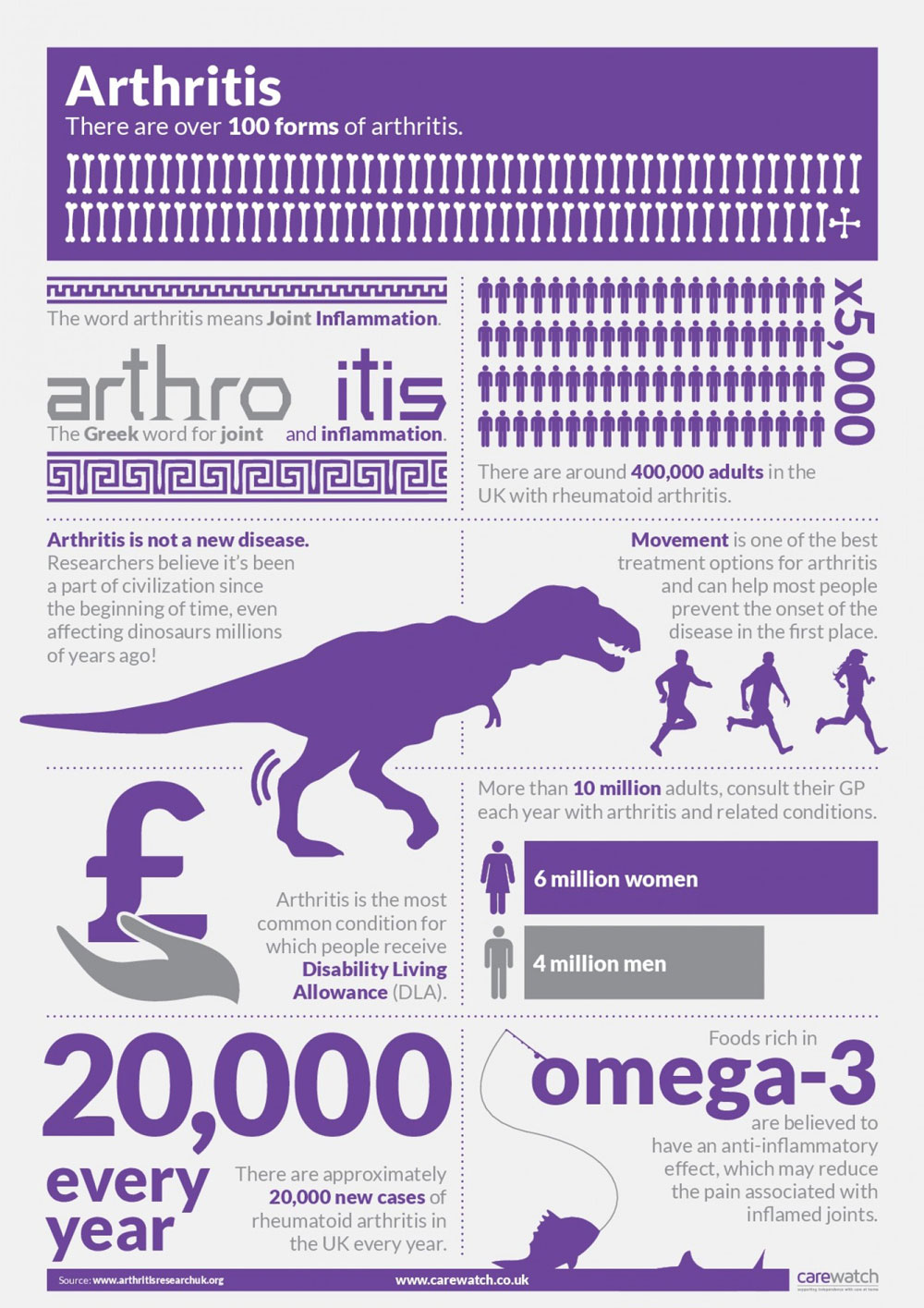
Infographic - Arthritis Apr 29th, 2014
Workers Comp Cost Containment Starts With Post-Injury Investigation Apr 27th, 2014
Employers often think they have completed their investigation of the new workers’ compensation claim when they have finished filling out the WorkCover WA Claim Lodgement Form (CLF) and First Medical Certificate; The information on the CLF is a good start on investigating a new injury claim, but it is not the only information that needs to be developed when investigating an injury claim.
Much of the information on the CLF – employee name, address, date of birth, social security number, and home phone number – can be taken right off the employee’s personnel file; Other information to complete the CLF– date and time of the accident, location of the accident, what happen, etc., can be obtained from the injured employee’s supervisor or department manager. Often the CLF is completed without the injury management co-ordinator for the employer ever talking to the injured employee. This is a major mistake.
Post-Injury Interview Should Be Thorough
The injury managment co-ordinator should interview the injured employee, in person if possible or by phone if an in person interview is not possible, to discuss the accident. The interview should include several important questions or topics:
- Exactly where in the workplace did the accident occur?
- Was the employee doing his/her regular job?
- How did the accident occur?
- Was a third party responsible for the injury? (Think Cost Recovery).
- Repeat the details of the accident to the employee to verify your understanding of the accident is correct.
- Confirm the accident occurred within the course and scope of employment.
- Ask the employee what the employer can do to prevent the accident from happening again.
- Obtain the names of all coworkers who witnessed the accident.
- Ask the employee to provide a detailed description of all injuries, including symptoms and level of pain.
- Ask the employee what is the medical provider’s diagnosis, prognosis, treatment plan and work restrictions. (Think Return to Work)
- Confirm the employee treated at the designated medical facility.
- If the employee has treated at an unauthorized medical provider, instruct the employee on the correct medical provider for any additional medical treatment.
- If the employee has the right to select his/her own medical provider, obtain the name of the medical provider along with the address and phone number.
- Ask the employee if they have ever had a prior injury. (This includes both work-related injuries and non-work related injuries). Later, after your discussion with the employee, compare their answers to their job application to see if their “new work injury” is a pre-existing medical problem.
- If the employee does disclose a prior work-related injury(s), obtain the name of the employer(s) and the date(s) of the prior injury(s).
- Discuss with the injured employee what work the employee is still capable of doing within the work restrictions set by the medical provider. (Think Suiitable Duties)
- Review with the employee what the medical management program will do to assist in their recovery.
- Reinforce the need for the employee to contact you following each doctor’s visit for the purpose of providing you with an update on the medical recovery and the work restrictions.
Good Information Creates Improved Work Comp Claim Outcomes
While this might seem like a lot of information to collect if the employee should be off work only for a few days or a few weeks, it is essential you do so. When the employer does not have a complete investigation and complete understanding of the medical care and progress, there is a much higher probability the injured employee will exploit the injury and being off work a few months or years rather than days or weeks.
Also, your investigation into the claim can often be essential in the prevention, or at least limitation, of medical treatment and lost work days due to pre-existing medical conditions. Plus, when employees know that the employer thoroughly investigates every injury claim, the incidents of fraudulent claims is greatly diminished.
Work Cover WA - Worker Compensation Claim Form Apr 27th, 2014
Work Cover WA - First Medical Certificate Apr 27th, 2014
Physical Activity Levels in Children Apr 26th, 2014
Physical Activity during childhood produces immediate and, long-term health benefits in adulthood. WHO international guidelines recommend that children participate in at least 60 minutes of moderate-to-vigorous physical activity (MVPA) daily. Worldwide, research has indicated that children are not achieving these guidelines, with estimates of activity levels varying both between and within countries. For example, 42% of children aged six to 11 years in the United States [16] participate in 60 minutes of MVPA daily. Similarly, in the United Kingdom (UK), objectively measured PA measurements indicate that just 51% of four to 10 year olds (33% of four to 15 year olds) meet the recommended guidelines. Achieving the recommended levels of PA per day is essential for the prevention and treatment of many health problems such as obesity. In particular, with evidence of tracking PA from childhood through adolescence and into adulthood, developing an active lifestyle from a young age may also produce long term benefits.
Being a member of a sports or fitness club, and, having an active favourite hobby were both positively associated with higher levels of PA. Exceeding two hours of total screen time and being overweight or obese were negatively correlated with higher PA levels. Children who were members of a sports or fitness group were almost twice as likely to be in the high PA group compared to children who were not. Exceeding 2 hours of totoal screen time reduced the likelihood of high PA by 44%.
Managing Stress Apr 23rd, 2014

10 proactive hazard identification methods Apr 23rd, 2014
Here are 10 methods you could adopt to identify health and safety hazards before an incident occurs:
- conducting pre-start discussions on the work to be carried out;
- encouraging workers to recognise and highlight hazards while performing work;
- carrying out safety inspections and audits of the workplace and work procedures;
- conducting job safety analyses (or similar task evaluation processes);
- monitoring, measuring and testing the working environment such as noise monitoring, electrical testing and atmospheric testing;
- analysing proposed new or modified plant, material, process or structure;
- conducting hazard (or risk) surveys;
- reviewing product information, e.g. safety data sheets, operating manuals; and
- researching publicly available data on hazards, e.g. newspaper articles, industry or safety regulator alerts; and
- looking at past incident and near-miss reports.
Reference:
7 Things We Can Learn About Aging Gracefully Apr 23rd, 2014
click for full story
The world's largest population of older healthy adults is on the Japanese island of Okinawa. And the last two people who held the title of world's oldest person (116 in both cases) were from Japan.
So what does Japan know that the Western world doesn't about longevity and aging? We'd broaden that to what does the East know that the West doesn't? Here are seven things we can learn from the East about aging:
- Healthy arteries don't just happen; you need to work at them.
- Yes, genes matter.
- It isn't just that they live longer; they live better.
- They not only exercise, but they do it as a community.
- The need to get things in balance is understood.
- A diet is what you eat for life; dieting is what occurs when you don't have a diet
- Naps are your friend.
How to manage an ageing workforce Apr 17th, 2014
In his Autumn statement last year, the chancellor of the exchequer set in motion plans to raise the state pension age to 70 for today's young people, on course to be the highest in the world. The question of whether people will need to work longer in the future is pretty much settled but there is still a lack of clarity about what work will be like for older workers of the future and how managers will oversee increasingly ageing workforces.
Answering the question of how to extend working life made a significant advance when the NHS Working Longer Review group reported the preliminary findings of its investigation into the impact of higher pension ages on the delivery of health services. This is the largest review of working practices in relation to age undertaken in the UK.
The outcome of their work is likely to prove seminal to the construction of a 21st century workplace bespoke to an ageing workforce for four reasons.
- Listen to the concerns of the staff
- Career progression
- A precious resource
- The need for dialogue with unions
Fight back against insurance premium increases Apr 15th, 2014

These recommendations together will give your control in the battle to minimize the cost of workers’ compensation.
Safety Program:
The lowest cost workers’ compensation claim is the one that never occurs. When an insurer is calculating your annual premium they review the frequency of accidents and the severity of the accidents that do occur, as well as the costs. A strong safety program will incorporate safety training for all employees, manual handling training, a job hazard analysis to identify and eliminate causes of accidents, work-site evaluations and inspections to prevent accidents, and a safety specialist or safety committee to keep safe practices at the fore-front of your work process.
Return to Work Program:
It is mandatory for your company to have an injury managment system and a company-wide return to work policy should be implemented. The return to work policy should be a part of every new employee’s orientation. It should be posted on the employee’s bulletin board and be discussed in staff meetings. All employees should know a job will be available to them as soon as they medically approved for light duties.
The company’s Injury Management Co-ordinator (IMC) should place a call to the medical provider the day of the initial medical treatment to learn the work restrictions provided by the doctor. The IMC should advise the doctor of the employer’s willingness to modify the employee’s job duties to comply with the work restrictions and be able to provide details of avaliable suitable duties.
Wellness Program:
An integrated health and wellness program will reduce the cost of workers’ compensation by reducing the impact of comorbidities on the injured employee’s recovery. The combination of unhealthy employee's and an aging population, with moves to increase the retirement age mean you will be increasingly hiring people with with one or a number of chronic conditions. By reducing obesity, diabetes, hypertension and physical deconditioning, an injured employee recovers faster from an injury, reducing both the amount paid for medical care and the time lost from work.
Get started with our free online LifeRISK Program.
Medical Cost Control Program:
In Western Australia, medical expenses make up ~16.0% of the total cost of worker comp. By directing the injured employee to a doctor with vocational medicine experience who understands the need to get the employee back to work as soon as feasible, you will eliminate unnecessary medical treatment and unnecessary delay in the employee returning to work.
From the moment of injury and Post-Injury Investigation, until the injured employee has reached maximum medical improvement, the course of the medical care should be managed. Initially, an IMC or occupational nurse can arrange the immediate first aid and any subsequent medical appointments. If the injury is severe, and the employee is going to be off work, the IMC or a preferred voc rehab provider can monitor and assist with coordination of medical care.
Line Supervisors - An Important role in RTW Apr 15th, 2014
Although there are many stakeholders in the RTW process, and employees supervisor has a pivotal role. A review of workers’ compensation systems in Australia revealed that injured workers nominated someone from the workplace as providing the most help with their RTW (16 %), third after their general practitioner (20 %) and their physiotherapist (19 %). Of that 16 %, nearly one-third (30 %) of injured workers nominated their immediate supervisor as the most helpful person at the workplace compared with occupational health and safety (OHS) officers (8 %), human resource (HR) staff (3 %) or RTW coordinators (3 %). However, 16 % of injured workers said their supervisor made RTW harder and these workers were less likely to sustain RTW.
Employee supervisors provide:
- modified work,
- interpret policies,
- assist with access to resources,
- monitor workers’ health and functioning,
- facilitate communication among stakeholders, and
- communicate positive messages of concern and support, while having intimate knowledge of the jobs available.
- The interface among upper management, rehabilitation and health care providers, coworkers, and the injured worker.
However supervisors frequently experience role conflict between their production responsibilities and the demands of the modified work program. Some do not have a good understanding of musculoskeletal disorders (MSDs) or the ergonomic principles underlying the selection of appropriate duties or how to modify duties to meet the medical restrictions. These problems may result in the supervisor either not adhering to restrictions set by the medical certificate or preferring the worker to be fully recovered before RTW, neither of which is desirable.
Johnston et al, 2014 put forward a model of the 10 competencies that should receive priority in any training delivered to supervisors. Supervisors need and seek support from experts in managing staff returning to work. This support can assist with complex cases, provide clarity to the supervisor’s role, and connect the returning worker to the services available within the organization. In large organizations this support may be available from in-house rehabilitation and RTW specialists but small to medium sized organizations may be disadvantaged by its absence.
- Managing and respecting privacy issues and medical and other conï¬dential information received
- Knowing the tasks and workload of the worker’s job
- Knowing what and how much the injured worker can and can’t do and how the injury impacts on the demands of the job
- (MHC) Managing privacy issues in terms of disclosure, e.g. with co-workers
- Being honest
- Being able to manage conflict
- Being able to deliver sensitive information, including information the injured worker doesn’t want to hear
- Being fair and just
- Communicating in a respectful and appropriate way
- Knowing their legal obligations as supervisors
Sports Performance Testing Apr 14th, 2014
Independent Medical Examinations and Specialist Assessment Apr 13th, 2014
Independent medical and Specialist examinations (IME's) can be an effective way to determine an injured worker’s medical status. But too often, they turn out to be a waste of money.
Here are a few tips for understanding getting the most from an IME:
- Before scheduling an IME, the claims manager and treating GP must know its purpose. Be specific about the details. Whether the issue is misdiagnosis, causation or degree of disability, provide medical reports, witness and injured worker statements, and other supporting materials.
- Find out the state’s laws and applicable treatment guidelines. Make a checklist of what needs to be done, how and when. Some states dictate timing and conditions of the IME. More often than not, IMEs occur too late in the process. Therefore, start considering an IME when the medical pieces of a claim are not fitting together and/or “red/yellow flags” are showing up.
- To ensure credibility, hire well qualified and highly respected doctors. Those with a relevant specialty tend to get more weight than generalists. Doctors with successful private practices, are affiliated with teaching hospitals or are involved in research are generally given more credence.
- IMEs related to returning an injured worker to the job should include specific job requirements (i.e duties registry/suitable duties registry) according to the employer, physician input and the employer’s efforts to assure return to work.
- Communicate clearly to appropriate parties throughout the claims process. No matter how much you follow the other steps, miscommunication can cause something to go wrong.
Return to Work Tips Apr 13th, 2014
Returning injured workers to work is simply the right thing to do. Return to work is as humane as providing immediate appropriate medical care because workers who do not return to the job face lower salary potential in the future. There are several reasons for this. Working is good for us both physically and mentally, and the longer workers are away from the job and feel disconnected from their employer, the harder returning to work becomes. At a basic level, successful employers maintain contact with injured employees and believe that finding work for them during recovery is important. They prepare for return to work before an injury occurs, set clear expectations, consistently monitor employees on modified duty and more.
Here’s more ideas from the experts:
Consider taking the long view. Since workers who spend years loading and unloading heavy objects are more likely to sustain an injury, consider developing career paths for blue-collar workers. Potential career progression jobs include fork life operator or inspector.
Create a Suitable Duties Registry before an injury occurs. Approach each department of your organization to find out what work can be done by someone on limited duty. Constantly update the job list. Each job should include the position’s physical demands to appropriately match the injured employee to the job.
Have a formal written early return-to-work policy. A 'written' injury management sytem is legislatively required in WA. Consider including language limiting the time frames for the light duty as well as cautioning how transitional duty must meet relevant medical restrictions.
Clearly communicate to employees about workers’ compensation. This is most clearly and transperantly done by a formal Injury Managment Policy.
After injury, contact the injured worker as soon as possible. When the immediate supervisor and Injury Management Co-ordinator learn of the incident or the claim, he or she should contact the injured worker within 24 hours. Assistthe employee with filing a workers’ compensation claim forms and tell workers they are missed and that accommodations will be made for a transitional job as soon as possible.
Involve the injured worker’s doctor when developing a modified duty job with multiple restrictions. Rather than merely telling the worker about the modified job, put together a team that includes human resources, the supervisor, engineer and employee to work together to anticipate potential glitches.
Informally gather the crew, supervisor, and the employee before putting him or her on transitional duty. This will make it easier to follow the doctor’s orders when everyone is aware of the worker’s restrictions as the employee works up to their MMI.
Ensure supervisors are accommodating rehabilitation plans by granting injured workers permission to elevate their feet, stretch and walk as recommended by the doctor.
To discourage re-injury, require managers to record workers’ activities when they return to the job. Include not only workers’ accomplishments but also tasks that they refuse. A detailed record of abilities and accomplishments could deter non-compliance and discrimination claims.
Encourage workers on modified duty jobs to spend their free time practicing safety exercises instead of sending workers home when they finish their work early. Injured workers can also get more safety training by watching videos or taking safety quizzes. Perhaps they can share what they learned at a safety meeting.
Arthritic knee solutions Apr 11th, 2014
CONSIDER the alternative to total knee replacement in young, active patients with arthritis.
Medial compartment arthritis of the knee causes pain and interferes with the activities of many physiologically young and active patients.
Treatment options for these patients are limited if they wish to stay physically active. Total knee replacement (TKR) is reliable at providing pain relief for these patients but it restricts their work and sporting capabilities considerably.
The main goal of a high tibial osteotomy (HTO) is to realign the leg to decrease the pain associated with arthritis.
In younger patients who wish to remain active, this improves function and slows arthritis progression. Older or less active patients may be satisfied with a TKR.

Art of War - Lessons for Sport Apr 11th, 2014
The Physical Genius Apr 10th, 2014
Cochrane Review - Childhood Obesity Apr 10th, 2014
Prevention of childhood obesity is an international public health priority given the significant impact of obesity on acute and chronic diseases, general health, development and well-being. The international evidence base for strategies that governments, communities and families can implement to prevent obesity, and promote health, has been accumulating but remains unclear. This review primarily aims to update the previous Cochrane review of childhood obesity prevention research and determine the effectiveness of evaluated interventions intended to prevent obesity in children, assessed by change in Body Mass Index (BMI). Secondary aims were to examine the characteristics of the programs and strategies to answer the questions "What works for whom, why and for what cost?"
AUTHORS' CONCLUSIONS
We found strong evidence to support beneficial effects of child obesity prevention programmes on BMI, particularly for programmes targeted to children aged six to 12 years. However, given the unexplained heterogeneity and the likelihood of small study bias, these findings must be interpreted cautiously. A broad range of programme components were used in these studies and whilst it is not possible to distinguish which of these components contributed most to the beneficial effects observed, our synthesis indicates the following to be promising policies and strategies:
- school curriculum that includes healthy eating, physical activity and body image;
- increased sessions for physical activity and the development of fundamental movement skills throughout the school week;
- improvements in nutritional quality of the food supply in schools;
- environments and cultural practices that support children eating healthier foods and being active throughout each day;
- support for teachers and other staff to implement health promotion strategies and activities (e.g. professional development, capacity building activities);
- parent support and home activities that encourage children to be more active, eat more nutritious foods and spend less time in screen based activities.


