P: (08)9965 0697 F: (08)9964 7528
News
Couch to 2k - HBF Geraldton RunFest Program May 20th, 2015
Next Dietitian Talk Monday 25th May 2015 at 12 noon. May 18th, 2015
Temika Lee's next Dietitian Talk is on Monday 25th May, 12 noon at Central West Health & Rehabilitation in Geraldton. This talk is free for gym members and people who are completing Central West Health & Rehab's Diabetes Management and Chronic Disease Prevention programs.
This talk covers: 
- Healthy Eating Habits
- Glycemic Index
- Fat Types and Cholesterol
- Recipe Modification Label Reading
Lumbar compression forces while lifting and carrying May 12th, 2015
In the construction industry, lifting loads is a frequent occurrence. Manual material handling (MMH), in terms of lifting is associated with an increased incidence of work-related back disorders.
To prevent work-related back disorders as a result of lifting, the maximum load mass to be lifted by one worker has been set at 25 kg in the Netherlands, and the maximum load for manually lifting is set at 50 kg when lifted by two workers. Loads above 50 kg should always be lifted mechanically (Visser et al, 2015). However, mechanical transportation is not always feasible and when not available the loads should be lifted by more workers (team lifting), while not exceeding 25 kg per worker.
The above study examined the lumbar compression forces of handling loads, which occurs daily at construction sites. It was found that a 50-kg two-worker lift resulted in higher mean and maximum peak lumbar compression forces compared with a 100-kg four-worker lift.
Carrying a load while stepping over an obstacle resulted in higher mean and maximum peak lumbar compression forces compared with carrying on level ground. The variability of the peak lumbar compression forces during the carrying tasks was higher while stepping over an obstacle compared to carrying on level ground for carrying 50-kg and 100-kg loads.
Compared to lifting, carrying a 100-kg load while stepping over an obstacle or up a platform led to a higher variability. Carrying a load up a platform resulted in the highest compression forces.
To reduce peak lumbar compression forces, lifting a fixed load mass with additional workers is advised. However, the benefits of additional workers are task-dependent (e.g., carrying vs. lifting). Additionally, the question remains whether the use of an additional worker is feasible in practice.
Two overall recommendations were made:
- Efforts should be made to prevent manual lifting and carrying of objects to reduce exposure of high compression forces during lifting and carrying.
- When mechanical transportation is not possible and loads are handled manually, carrying routes should be free of any obstacles to be overcome.
Australian Doctor - Diabetes Strategy urges GP payment overhaul Apr 15th, 2015
Pay-for-performance incentives that would see GPs paid on the basis of how many patients they screen and treat for diabetes form a central plank of a new national diabetes strategy.
The National Diabetes Strategy consultation paper states that fee-for-service payments are not working for diabetes and should be supplemented by payments based on quality and outcomes measures.
The Federal Government's paper, released on Wednesday, lays out five key target areas for change, which include:
- increasing the number of people who are screened and diagnosed early with diabetes
- boosting the number of patients with diabetes receiving structured management programs in primary care
It notes that currently only 18% of patients with diabetes had an annual cycle of care completed by a GP, and suggested that this could be improved by linking performance benchmarks to reimbursement
"The fee-for-service model does not incentivise long-term follow-up or the proactive care of people with chronic conditions. As such, more innovative funding models are needed that combine fee-for-service reimbursement with other payment types, such as population-based payments and quality-based payments," the consultation paper said.
"The government could consider exploring (potentially through demonstration projects) an innovative combination of payment models, such as pooled funds, ‘medical homes,' capitation payments, pay for performance, and pay for quality and outcomes based on performance indicators."
The paper also suggests new funding models for allied health professionals.
Among the other proposals are a national program for detecting prediabetes and early diabetes based on the AUSDRISK tools, and programs based in Primary Health Networks to encourage annual screening for complications
The National Diabetes Strategy should also include measures to improve access to medications and devices such as insulin pumps, and encourage uptake of the PCEHR by people with diabetes, the consultation paper suggests.
The proposals have been released by the National Diabetes Strategy Advisory group, set up by former health minister Peter Dutton in 2013, which is led by endocrinologist Professor Paul Zimmet and former MP Judi Moylan.
It is accepting feedback on the proposals until 17 May and will release a final National Diabetes Strategy in late 2015.
The proposals have been backed by RACGP resident Dr Frank Jones, who said they were in line with the college's newly released new primary healthcare funding model that proposes a move away from fee-for service funding.
"[The Diabetes Strategy proposal] basically reinforces our viewpoint that you can't look after patients with chronic disease with the Medicare model that we have," he told Australian Doctor.
Dr Jones said the RACGP model would retain fee for service for acute episodic care, but would introduce patient enrolment and replace PIP and SIP incentives with practitioner and practice-directed loading payments based on "comprehensiveness" and complexity of care.
The new reimbursement would recognise the ongoing work that GPs did with patients such as those with chronic and complex diseases, according to Dr Jones.
"We really believe that GPs who provide quality care ought to be recognised," he said.
Pacing your Lifestyle and Exercise Apr 14th, 2015
“Pacing is an active self-management strategy whereby individuals develop self-efficacy through learning to balance time spent on activity and rest for the purpose of achieving increased function.”
Jamieson-Lega et al (2013)
Pacing involves learning to balance your time spent on exercise and activities, to avoid overactivity or underactivity. It is about being able to manage your chronic pain more effectively, to achieve a balance between rest and activity. This enables you to perform meaningful activities with less pain interference.
When you start an exercise program, you may struggle to adopt the right pace and technique in developing your fitness training. As a result, exercise can feel like a struggle. If you’ve experienced difficulty sticking with your exercise regime, the problem is likely to be one of pacing judgment and intensity:
a) Starting your exercise too quickly and paying the price later on
b) Completing sessions too conservatively and feeling you’ve got a lot more left in the tank
The solution is learning how to evaluate your training intensity and match it to your session so that you get maximum training benefits — and importantly, enjoy your training sessions.
“After having a serious illness a few years ago, and not being able to exercise without pain, I was unsure of how to begin an exercise plan without making my symptoms worse. I then realized that if I paced myself, I might be able to exercise successfully without the symptoms getting worse. I changed my thought processes from trying to lose weight and getting fit, to relieving the symptoms of my chronic pain. I started at a very slow pace, not pushing myself at all, a pace that I could do on my worst days, and then as it became easier, with no pain I increased the pace of my exercise program” Anonymous
Rhianne Turner Physiotherapist
Pacing your Lifestyle Apr 14th, 2015
“Pacing and balancing tasks become skills that can assist with managing chronic pain”
 It is important to prioritise activities so that the most important tasks get done first. This way if you are unable to finish every task, then at least the most important tasks are done. Also, try to leave yourself plenty of time to complete each task. Pacing your lifestyle will provide you with an effective means of achieving your goal, provided you are realistic in choosing the priorities in your life.
It is important to prioritise activities so that the most important tasks get done first. This way if you are unable to finish every task, then at least the most important tasks are done. Also, try to leave yourself plenty of time to complete each task. Pacing your lifestyle will provide you with an effective means of achieving your goal, provided you are realistic in choosing the priorities in your life.Performing one major task in small steps each day can lead to feelings of achievement and build your coping strategies. This will take time and patience. Try not to compare yourself to what you used to be able to achieve before the onset of chronic pain, this may not be realistic initially.
Following a routine of less pleasurable activities/chores followed by enjoyable activities can also assist in the pacing process, rewarding yourself for your achievements.
WHAT TO AVOID
Chronic pain commonly leads to ‘Good days and Bad days’. It is important not to use good days for going hard at physical activity – as you will surely feel those bad days and need some time to rest and recover.
An increase in muscle pain is to be expected as you are using muscles and joints in new ways, known as Exercise Induced Muscle Soreness (EIMS).
Boom – Bust Approach is when a person does too much all at once, crashes, rests, starts to feel better and does too much once again. If activities or exercises are not spread out, a boom-bust cycle will occur. At times this may be inevitable; however when Boom-Bust approaches become habitual it can result in exhaustion, sleep disturbances, insomnia, appetite and weight changes, or mood swings. You should learn to recognise contributors such as fear avoidance, attitudes and beliefs.
Watch out for Boom-Bust signs as they can significantly increase pain levels, such as:
a) being highly motivated to achieve your goal that you significantly increase pain levels
b) being apprehensive about what may happen if things don’t get done
c) having a high number of commitments or responsibilities to meet
10 TIPS FOR SUCCESSFUL PACING

- Be consistent. Be persistent. Be patient with yourself.
- Choose something you enjoy
- Have a realistic timeframe, gradually making the activity harder and changing the environment (from walking on level ground to walking uphill or on the beach)
- Pace your activities, even on bad days (avoid good day, bad day behaviour)
- Have rest periods
- Listen to your Body: The body sends us signs and signals when it is being overworked, so it is important to balance rest and activity
- Stick to your designated time limit: use a timer and be disciplined in starting and stopping activities
- Use a diary to record your progress so you can pace accordingly and measure your achievements
- Avoid too large of an increase in activity to avoid a ‘Boom-Bust’ approach to exercise
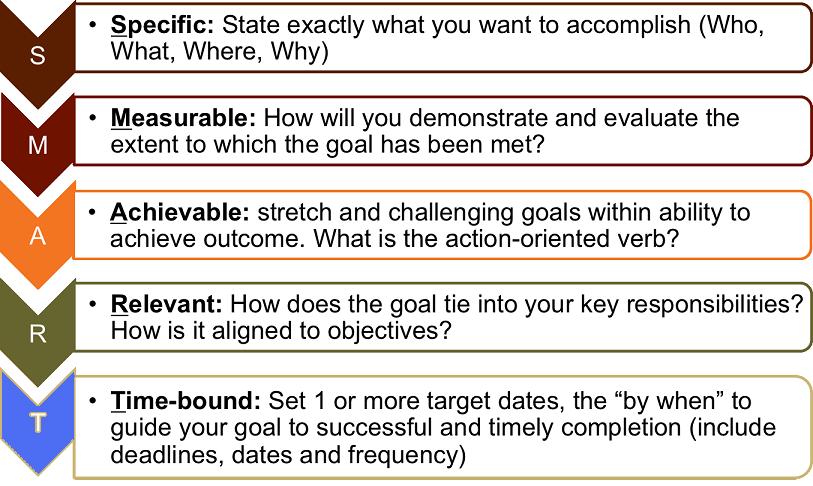
- To improve your pacing, undertake a little more each week, gradually building up physical activity over time. It is important to set SMART goals to pace yourself so that these realistic goals can be met
Rhianne Turner Physiotherapist
Infographic- SMART Goals Apr 14th, 2015
Insurers won’t run PHNs Apr 13th, 2015
PRIVATE health insurers will not take roles in running new Primary Health Networks despite reports describing them as partners in successful PHN consortiums.
Health Minister Sussan Ley (pictured) on Saturday announced the successful tenderers for 28 of the 31 PHNs, which are to replace Labor’s 60 Medicare Locals as of 1 July.
Ms Ley’s media release said many of the successful PHNs were “consortiums harnessing the best skills and knowledge from a range of sources, including allied health providers, universities, private health insurers and some of the more successful former Medicare Locals”.
Adding to the impression that the insurers had managed something of a coup, a weekend news report said the Abbott government had “handed control” to a range of groups including the two major health insurers HCF and Bupa.
Giving a specific example, the News Ltd report said the North Brisbane PHN would be “run” by Metro North Brisbane Medicare Local (MNBML), together with Metro North Hospital and Health Service, Children’s Health Queensland Hospital and Health Service, Telstra Health, AMA Queensland, UnitingCare Health, and the two insurers.
However, Medical Observer has confirmed that only four of the 28 successful bids had any involvement with private health insurers, and their roles are strictly as support players.
MNBML CEO Abbe Anderson said HCF and BUPA were just two of many groups that had backed the successful application from her organisation.
“While MNBML has the support of a wide range of key participants – including those listed – I think we had over 30 organisations that provided us with letters of support and endorsement in our application,” Ms Anderson toldMedical Observer.
“But the PHN itself will be governed and managed by the same organisation that has been running the ML since its inception.
That organisation – Partners 4 Health, the registered trading name of MNBML – has been in place for four years and is very much a “grassroots” outfit, she said.
“It has a local membership structure of over 20 organisations, all of which represent local clinicians and community groups, and that will be complemented by the formation of new clinical councils and community adviser groups,” Ms Anderson said.
She said private insurers shared the same imperatives as hospitals and primary care groups - trying to keeping people well and out of hospitals - adding they were in conversation “about the types or program we want to see".
“In our experience, private health insurers are very willing to look at chronic disease programs that benefit everyone, that aren’t just aimed at their members,” she said.
But Ms Anderson did not see any risk of a push for preferential treatment of private health fund members.
“I honestly see everyone working very collaboratively together, and I guess that’s one of the key reasons why we need the voices of GPs and other clinicians in the planning of these models, to ensure we don’t end up with systems that somebody will lose out on.”
Dr Marcus Tan, a director of WA Primary Health Alliance, which has landed contracts for three WA PHNs, said his organisation saw a similar need to take “a very collaborative approach” including input from the same two insurers.
“This is recognition of the need for an integrated healthcare system to have government, non-government and private involvement,” he said.
“The private health insurers have signalled their interest in chronic care, for example – but they are not formally part of the organisation.”
The Alliance was formed from Perth Central & East Metro ML, Goldfields-Midwest ML, Perth South Coastal ML and Fremantle ML, with endorsement from Bupa and HCF among others.
Dr Tan said he thought the Perth North, Perth South and Country WA PHNs would make the 1 July start date because much of the established resources and infrastructure of the Medicare Locals would be transitioned into the new networks.
In Victoria, the Grampians and Barwon South West PHN was also named as having a private health-fund partner aboard.
But Jason Trethowan, CEO of Barwon Medicare Local, which will manage the new PHN covering western Victoria, said the association with locally based private health insurer GMHBA was entirely without conflict.
“Our Medicare Local is the company that will change its name and constitution to establish the PHN for western Victoria,” Mr Trethowan said, adding GMHBA and the four local hospital networks would all be critical in the rollout.
“But there’s no deals, no role in governance, no seats on boards, no interference with the running of the PHN,” he said.
“Where there are areas where [GMHBA] can support us or work with us, then we would do so.
“It was important in our submission to show we had a strong buy-on from Deakin University, four major hospital networks and also a health fund that has most of its members in our footprint.”
South Eastern NSW PHN is the fourth new entity identified by the minister’s office as having private-insurer backing.
The managing organisation is Coordinare Limited, formed by the Illawarra Shoalhaven ML, supported by the University of Wollongong and Peoplecare, a member-owned, not-for-profit health fund based in Wollongong.
Australian Doctor - Axed preventive health program showed promise Apr 2nd, 2015
Australia’s national preventive health program was showing promising results before it was scrapped in last year’s budget, according to a belatedly released Department of Health report.
The National Partnership Agreement on Preventative Health (NPAPH) was introduced as a COAG initiative under Labor in 2008 with programs to reduce smoking rates, combat excess alcohol intake, boost physical activity and improve diet.
The Coalition axed the program in the 2014 federal budget and diverted the savings of $368 million over four years to the Medical Research Future Fund.
However, an independent evaluation report released under a Freedom of Information request showed that six months before the partnership agreement was abandoned, the government was told the program "appears to be a sound, evidence-based and highly appropriate investment in preventive health".
"Overall, approaches have been based on effective health promotion principles and best-available evidence, and there is a judicious mix of innovative and evidence-based strategy," the report authors said.
"Available evidence indicates that implementation is on track, and that some states and territories are achieving a good level of reach into target groups."
The programs funded by the NPAPH included the Healthy Children Initiative, the Healthy Workers initiative, the Measure Up campaign, the National Tobacco campaign, and the Healthy Communities Initiative.
The report was finalised in January 2014, when the future of the NPAPH still looked bright.
"While it is too early to reach conclusions on the likely extent that the NPAPH will achieve its longer term outcomes ... the current evidence of reasonably effective partnership processes and successful implementation of initiatives indicates that considerable progress is being made in the right direction," it concluded.
This week, 11 peak health groups raised concerns about the axing of a wide range of preventive health programs.
"We are particularly concerned about the future of the Close the Gap Indigenous Chronic Disease package, which aims to prevent chronic disease including GP services, medications and tackling smoking. The new Primary Health Networks will not be able to pick these critical programs up as they have barely been established yet," said Lisa Briggs, CEO of the National Aboriginal Community Controlled Health Organisation.
Federal Minister for Health Sussan Ley could not be reached for comment.
Realising the Health Benefits of Work for all Australians Mar 31st, 2015
 Realising the health benefits of work for all Australians requires a paradigm shift in thinking and practice. It necessitates cooperation between many stakeholders, including government, employers, unions, insurance companies, legal practitioners, advocacy groups, and the medical, nursing and allied health professions.
Realising the health benefits of work for all Australians requires a paradigm shift in thinking and practice. It necessitates cooperation between many stakeholders, including government, employers, unions, insurance companies, legal practitioners, advocacy groups, and the medical, nursing and allied health professions.The family doctor is best placed to advise and educate patients that, in most cases, a focus on return to work is in the best interest of the patient – for both their future and quality of life and that of their family.
Return to work is not possible for everyone, but certifying time off work – particularly when absence is long term – can have significant side effects, including increased rates of overall mortality, poorer physical health and poorer mental health and psychological wellbeing.
The following document is a consensus statement from the Australian Faculty of Occupational and Environmental Medicine. It highlights the importance of a trusted GP in assisting employee's to return to work.
Despite all of the above, research continues to show that many GPs are unlikely to recommend alternate duties for injured workers, and many GP’s who suggest a ‘special interest’ don’t always follow these best practice guidelines.
I hope that the above highlights the significant benefits to be gained from offering employees a 'trusted' GP and Injury Management Service.
Reassuring Employees About Low Back Pain Mar 28th, 2015
In the 2012-2013 Australian Workers Compensation Statistics 22% of serious claims were due to back pain and some 33% of serious claims were caused by muscular strain while lifting or handling objects.
Despite trends showing increasing use of advanced imaging tests, opioids, and invasive surgical and interventional procedures, with attendant increases in costs, the prevalence and burdens associated with back pain appear to be on the rise.
In fact, there is growing evidence that those who suggest a ‘special interest’ in managing back pain often provide less appropriate treatment recommendations. These providers often hold alternative beliefs regarding the association of pain and activity that influence their practice behaviour.
For example, the presence of common degenerative findings on spinal imaging poorly correlates with the presence of and severity of back pain or the likelihood of developing chronic disabling symptoms. Rather, predictors of chronicity are primarily psychosocial.
For this reason back pain is best understood as a complex biopsychosocial condition. Many other factors besides the employee's medical condition (e.g. acute back pain) affect outcomes– e.g. organizational, work-environmental, and social.
Most acute back pain improves substantially within the first 4 weeks. However, a small proportion of patients with acute back pain go on to develop chronic disabling symptoms. Such patients often are refractory to treatments and account for the majority of the costs associated with back pain. Preventing the transition from acute to chronic low back pain is therefore an important goal of current evaluation and management strategies.
The above paper provides a 2 page summary of evidence regards how best to approach the employee with acute back pain to alleviate patient worries and fears. This along with evidence based acute injury management assist in preventing the transition from acute to chronic low back pain.
Medical Observer - Better use of healthcare professionals is vital for a sustainable Medicare Mar 28th, 2015
Removing barriers to physiotherapists referring patients directly to medical specialists with a Medicare rebate, instead of requiring a GP referral, would achieve better patient-centred care, as well as over $13 million in savings to Medicare each year. This would also reduce out-of-pocket payments for patients by more than $2 million per year.
Other sustainable measures that would improve healthcare for patients and save money include:
- Physiotherapists leading screening clinics to triage surgery patients.
- Better supporting advanced scope physiotherapists in emergency departments to deal with patients with simple but urgent musculoskeletal injuries that are currently contributing to the burden on ED doctors. This has been shown to reduce patient waits, and helps move patients out of hospital more quickly.
- Enabling physiotherapists with additional qualifications and endorsement to prescribe medications within their scope of practice. The Medicare co-payment would have made access to primary care even more difficult for people who could least afford it.
The APA’s solution to improve the use of physiotherapists who are highly qualified and experienced primary health professionals to undertake these practices will ensure better patient-centred care and relieve pressure on the healthcare system.
The APA’s pre-budget submission for 2015–16 details APA’s recommendations on the referral to specialist issue. It is available online Click here.
The APA is the peak body representing the interests of Australian physiotherapists and their patients. It is a national organisation.
Cris Massis is CEO of the Australian Physiotherapy Association.
Many Reap Rewards in Wellness at Work! Mar 27th, 2015
Australia’s working population is becoming sedentary and workers are being asked to put off retirement and work longer hours.
TWO out of every three Australian adults have at least three or more risk factors for cardiovascular disease, diabetes and chronic kidney disease, according to a new AIHW report.
Employees with a cluster of seven heart disease risk factors have an average annual cost of ~$2640.00 more than employees with no modifiable risk factors.
Employers have a choice, proactively promote health promotion programs or expect to pay more in direct and indirect health related costs.
Workers spend a large proportion of their waking lives at the workplace and are a captive audience for any health promotion intervention.
We recognise that you, the employer, have extensive experience in ensuring the wellbeing and health of your staff. However there are times when it could be helpful to access the insight and expertise of a trusted partner to tailor services to your organisation and employee's needs.
Click to download copy
Our team of allied health professionals from a wide range of backgrounds give the perfect know-how and skills base to provide such an intervention in a proficient and energetic manner.
Medical Observer - Nine reasons why Australia needs to improve preventive health! Mar 25th, 2015
TWO out of every three Australian adults have at least three or more risk factors for cardiovascular disease, diabetes and chronic kidney disease, according to a new AIHW report.
Multiple risk factors were also prevalent among Australians who already had one of the conditions.
“For people with diabetes, nearly all adults (94%) had three or more risk factors, and for CVD and CKD, 84% and 77%, respectively, had three or more risk factors,” AIHW spokesperson Sushma Mathur said.
NINE FACTORS FOR ILL HEALTH
1. Just under a third of all adults have hypertension (including 22% with uncontrolled hypertension).
2. Almost two-thirds are overweight or obese, and 3% have impaired fasting glucose.
3. Over half the population is not active at all or insufficiently active.
4. One in six people smoke daily and one in five surpass guidelines for lifetime alcohol risk.
5. A third of Australian adults have high LDL-cholesterol, and 63% have dyslipidaemia.
6. People with cardiovascular disease are more likely to have uncontrolled hypertension (2.1 times), be overweight or obese (1.3 times), have dyslipidaemia (1.3 times) and be inactive or insufficiently active (1.2 times) than those without CVD.
7. Almost all adults (95%) do not eat the daily recommended two serves of fruit and five serves of vegetables.
8. People with type 2 diabetes are twice as likely to have uncontrolled hypertension, be overweight or obese (1.5 times), and have uncontrolled dyslipidaemia (1.2 times) than adults without the disease.
9. People with CKD are more likely to have uncontrolled hypertension (1.9 times), or have blood glucose levels ≥6.1 mmol/L (2.8 times) than adults without CKD.
Australian Doctor - Legal fallout follows hike in bariatric surgery Mar 23rd, 2015
The rise in bariatric surgery has seen it become a 'medicolegal hotspot' with many patients harbouring unrealistic expectations and little understanding of the high complication rates for the procedure.
The majority of claims now being made focused on informed consent, negligent performance of the surgery and inadequate post-management and follow-up, Janine McIlwraith (pictured), principal lawyer at Slater and Gordon, told last week's Medico Legal Congress in Sydney.
Patients also needed to know the surgery was "not a panacea and just part of a solution to weight loss", she said.
"They need to be committed to lifestyle modifications after surgery, and they need to be aware of complications and their frequency."
Patients tended to be well-educated and financially well-off but expected unrealistic outcomes, so consent procedures needed to be robust, she said.
The number of procedures has increased dramatically - from just 500 in 1998/99 to over 17,000 in 2008/9. About four in 10 procedures resulted in complications, Ms McIlwraith said.
A Medical Services Advisory Committee report in 2012 said bariatric surgery should be performed as part of a multidisciplinary effort to improve long-term outcomes.
However, very few patients were receiving that kind of care, Ms McIlwraith said, with most patients visiting solo practitioners.
The spike in claim numbers for bariatric surgery could simply be the result of a rise in procedure rates, she said, "but there may be other causes worth investigating".
Timing in RTW is everthing - What Next Mar 21st, 2015
Following on from the AIA paper, evidence from industry experts overwhelmingly supports early rehabilitation and RTW programs are a winning combination for all involved.
Concord General Hospital, Sydney is a self insurer, who in 2003-4 found themselves with a huge number of open claims (~300), and a spate of very difficult cases who went on to have chronic pain syndromes. The organisation felt they were failing injured workers and that something needed to change.
After significant internal investigation, the consensus was that the first 4 weeks after an incident/injury was the answer, – after that you start to lose control! They instigated a rapid assessment and early intervention process, which included an assessment psychosocial risk (i.e. Yellow Flags). The idea was that high risk individuals needed to be identified in the first week/s. Nothing different needed to be done; only it needed to be done earlier. It was also important that a trusted GP was in control of the whole process through consultation and approval.
Along with aggressive acute injury/illness management, return to work planning for high risk individuals was commenced from the day of injury in the form of planning, discussion and communication between injury management co-ordinators, health professionals (GP and Physiotherapist) and employee supervisors.
Key Points of Concord Case Study:
- There is a significant difference between the 20% in the “high risk” category and the other 80% who manage pretty well with ‘usual care’.
- Psychosocial risk factors (i.e. ‘Yellow Flags’) predict the cost of a workers compensation claim within 48 hours regardless of what or where the injury occurs.
- The provision of an early and aggressive assessment and intervention, lead by a trusted GP can reduce costs in high risk claims.
For successful RTW timing is everything! Mar 21st, 2015
Evidence suggests the longer the delay to rehabilitation and RTW planning following a workplace injury, the smaller the chances of a successful return to work outcome become. The following posts continue our focus on providing information to allow injury management co-ordinators to feel comfortable taking greater control of RTW processes.
DELAYS IN COMMENCING WORKPLACE BASED RETURN TO WORK
AIA Australia is a life insurance specialist trusted to protect more than 2.5 million Australian lives. AIA Australia is committed to helping people improve their health and therefore is a strong believer in workplace rehabilitation and the power it has, where health conditions permit, in getting people back to work – and therefore a full life – faster.
In August 2013 AIA produced a paper titled “A critical equation: balancing Australian worker health and company wealth” that noted in terms of physical conditions, as the number of days off work increases, the chances of successful return to work significantly decreases:
These are fairly sobering figures and are cause for alarm given a number of employers continue to take a ‘return when you are fully fit attitude’ to work related illness and injury.
WHY ARE DELAYS AN ISSUE?
Work is a determinant of health, both physical and psychological. The longer a person is away from work for an unplanned (or unmanaged) absence the more their health can potentially suffer.
Comcare engaged a consultant to conduct research into delays in providing rehabilitation or return to work assistance for their injured employees, after they identified a trend for employees injured at work to stay off work for long periods (6-12 weeks in majoity of cases)
The results were published in the paper “BODY STRESSING INJURIES: Key messages for rehabilitation providers”. One of the things the Consultant found in their analysis was in most cases, RTW assistance was not provided until after the normal recovery period for the injury. Consequently by the time assistance was offered it was often no longer appropriate.
The issue here is once a body stressing injury progresses beyond 12 weeks of incapacity it becomes a ‘chronic’ injury that is much harder to manage and rehabilitate due to numerous psychosocial issues. Equally with psychological injury claims there is often deterioration in the person’s mental status the longer they are away from work.
Amongst other findings, this report promoted that early recovery and return to work involves effective management of an injured employee by their employer and needs to commence as soon as practicable after the injury occurs and preferably before any claim for compensation is made.
Video - Diabetes Australia Healthy Eating Mar 20th, 2015
High Performance Jump Program Mar 10th, 2015
Day- Tuesday

Location – Central West Health and Rehab
Time – 4:00pm
Training focus – Jump Strength
Maximal strength determines jumping height. When trying to improve jump height athletes should focus on maximising strength development.
Day – Friday
Location – Central West Health and Rehab
Time – 4:00pm
Training focus – Jump Plyometrics
Plyometrics include performance of various types of body weight jumping-type exercise, like drop jumps (DJs), countermovement jumps (CMJs), alternate-leg bounding, hopping and other SSC jumping exercises. Plyometrics are a powerful tool for improving jumping performance.

Start Date: Tuesday; 21st of April 2015
Click for Registration Form
Payment required at initial physical assessment
Registration Form Mar 10th, 2015
Dietitian - 3 Day Food Diary Mar 9th, 2015
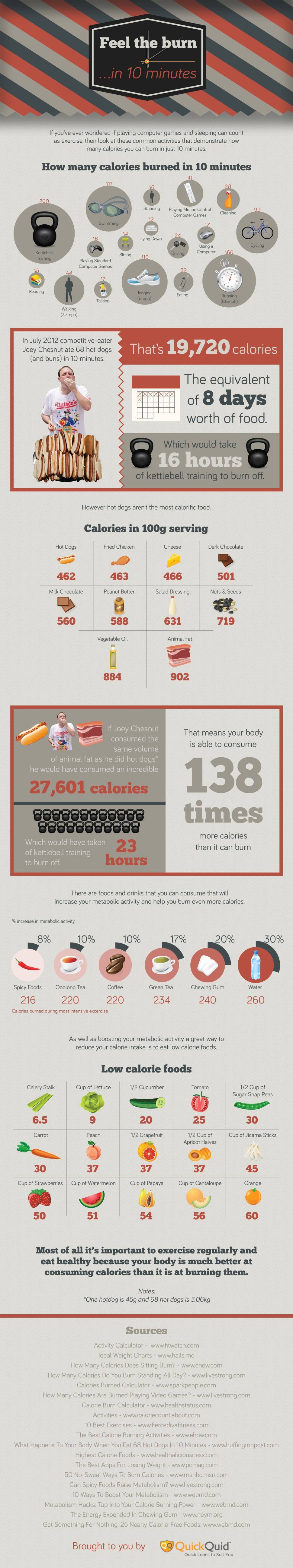
Infographic - Calories Burned in 10 minutes! Mar 9th, 2015
Test - Google Forms Mar 8th, 2015
This post is a test run of embedded Google Form data in News Post.
Medical Observer - Allied health keeps patients out of hospital Mar 7th, 2015
6th Mar 2015
Declan Bowring
STROKE, diabetes and osteoarthritis patients could avoid unnecessary hospital treatment with greater investment in allied health professionals, a new report says.
The report, produced for Services for Australian Rural and Remote Allied Health (SARRAH), found evidence that hip and knee replacements and diabetic limb amputations could be avoided and thousands of hospital beds freed up with targeted care by allied health teams.
“This report the first of its kind in Australia, has demonstrated the huge cost savings and patient benefits that Australia could achieve,” SARRAH CEO Rod Wellington said.
“It exposes the myth that allied health is an optional extra in healthcare.”
The report cited cases including:
- A 64% drop in diabetic limb amputations and a 24% decrease in hospital stays after treatment by podiatrists under the Queensland Diabetic Foot Innovation project.
- A 15-month reduction in the waiting list for joint replacement surgery at Melbourne’s Alfred hospital after triaging by physiotherapists.
- Fifteen per cent of osteoarthritis patients removed from the joint-replacement waiting list at a Sydney hospital after treatment by a multidisciplinary team.
- A 37% prevention rate in the incidence of diabetes among 2241 high-risk participants in eight international trials after intervention by dietitians, physiotherapists and exercise physiologists.
- Stroke care focusing on speech pathology in the NSW Illawarra region prevented 45 emergency presentations, 49 hospital admissions, 188 readmissions and saved 2808 bed days.
The report emphasised the value of physiotherapists, occupational therapists and speech pathologists in improving the function and independence of stroke patients.
Executive officer of Allied Health Professions Australia, Lin Oke, said affordability was a problem, noting Medicare Chronic Disease Management rebates for allied health services were “extremely limited”.
“The rebate of approximately $50 is based on a 20-minute service, regardless of the required length of the appointment with the allied health professional,” Ms Oke said.
“So many Australians just cannot afford the services which would keep them away from hospitals and surgical procedures.”
The report found a significant lack of access to allied health for rural patients, with only 14% of registered allied health professionals working in rural areas.
More than 1000 deaths from diabetes in rural areas could have been prevented if the mortality rate matched that of urban areas. In very remote areas, diabetes was the second-highest cause of death.
Independent MP for Denison, Andrew Wilkie, used the report’s findings to blast the Tasmanian government for cutting allied health staff in the state.
“To sack these vital front-line workers who can get people home from hospital sooner and prevent elective surgery is complete madness,” Mr Wilkie said.
“These workers are worth their weight in gold because they save hospitals money.”
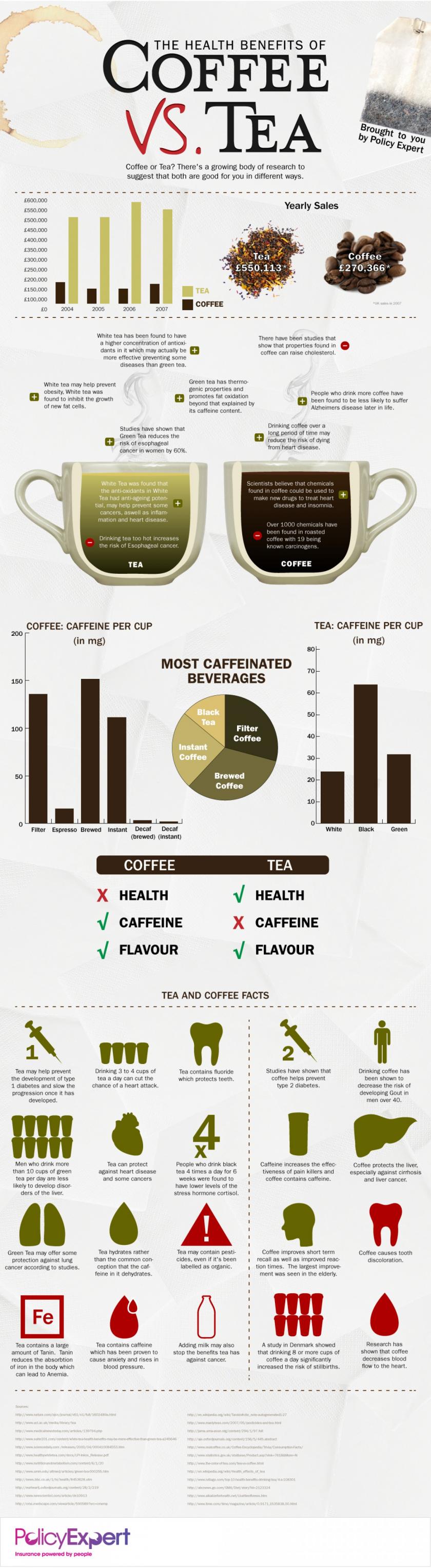
Infographic - Coffee Vs Tea, What is healthier? Mar 4th, 2015